Surgery is often considered for women with stress incontinence who fail to respond to conservative therapy.
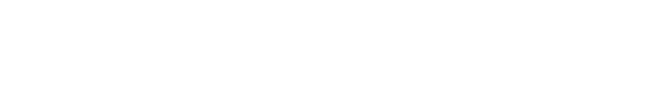
The flow chart below details the surgical options for women with stress incontinence that do not respond to pelvic floor muscle training.
Burch Colposuspension (Mesh free, native tissue surgery)
There are various surgical options for women with stress urinary incontinence who have not responded to physiotherapy or medications. A Burch colposuspension is an operation that has been used for more than 50 years with good long-term success rates of 80-85%. This surgery avoids the use of mesh (non-mesh or mesh free incontinence surgery). Dr Carey usually performs this by laparoscopy (keyhole) or robotic assistance. Dr Carey is highly experienced at performing the laparoscopic Burch colposuspension having performed this operation for more than 20 years.
What happens during surgery?
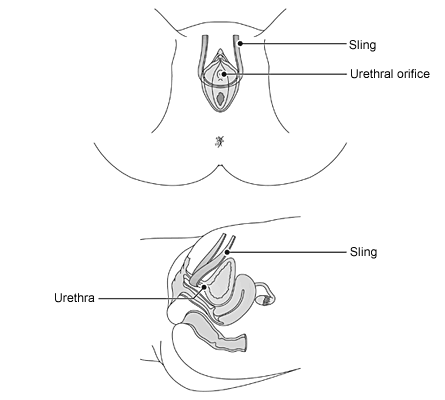
The Burch operation requires a full (general) anaesthetic and takes about 30 to 40 minutes to perform. Dr Carey usually performs this surgery by laparoscopy or with robotic assistance through small 0.5 to 1 cm incisions in the abdominal wall. Stitches are placed on each side of the urethra and into a ligament on the pubic bone (Copper’s ligament). This supports the urethra and prevents stress incontinence from occurring. At the end of the operation the inside of your bladder is looked at with a medical telescope to check that there is no bladder injury. A catheter is then inserted into the bladder to drain urine and remains in place over night. The Burch operation can be performed in combination with other procedures such as surgery for prolapse.
The illustrations above demonstrate the Burch operation. Sutures are used to re-support the urethral from Cooper’s ligament. This surgery avoids the use of mesh and is done by Dr Carey using laparoscopic or robotic assistance.
Pubo-vaginal Sling (Mesh free, native tissue surgery)
The Pubo-vaginal sling is an operation that has been used for many years with good long-term success rates of 80-85%. This surgery avoids the use of mesh (non-mesh or mesh free incontinence surgery). Dr Carey usually performs this surgery in more complex cases such as when other operations for stress incontinence have failed.
What happens during surgery?
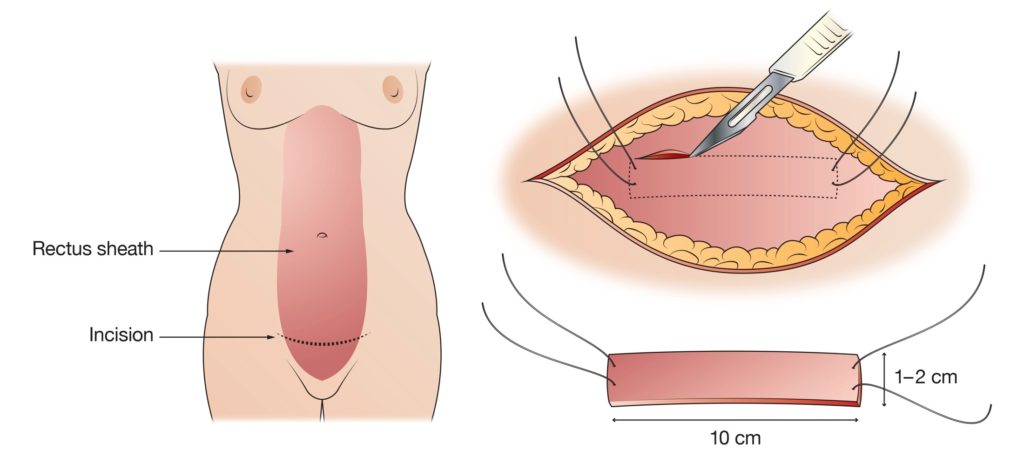
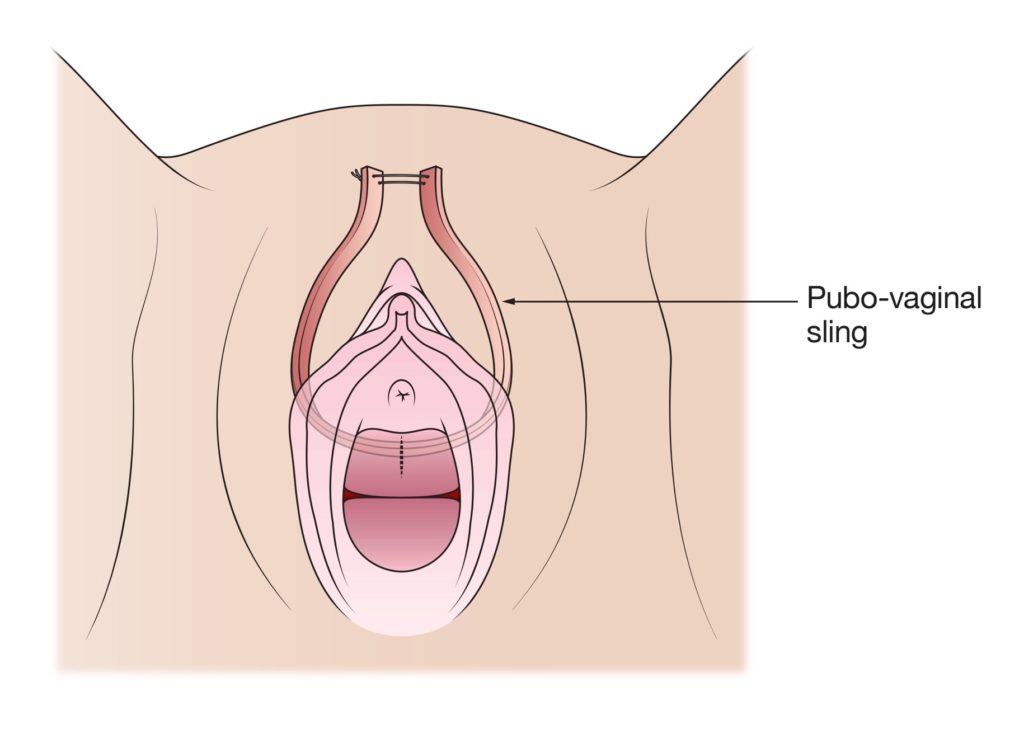
The Pub-vaginal sling usually requires a general anaesthetic but can also be done with a spinal anaesthetic. Surgery takes about 30 to 40 minutes to perform. The surgery is performed through an incision in the lower abdominal wall and a small incision in the vagina. The sling is taken from the rectus sheath in the lower abdominal wall and placed under and around the urethra through the small vaginal incision. The ends of the sling are tied over the rectus sheath. This supports the urethra and prevents stress incontinence from occurring. At the end of the operation the Dr Carey looks inside your bladder with a medical telescope to check to make sure there is no bladder injury and a catheter is inserted into the bladder to drain urine that remains in place over night.
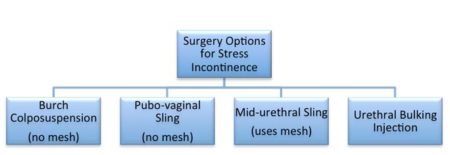
The illustration below demonstrates creating the sling from tissue (rectus sheath) in the lower abdominal wall.
The illustration below demonstrates the sling in position supporting the urethra.
Mid-urethral Sling (Mesh surgery)
The most widely used operation for stress incontinence is the mid-urethral sling procedure, often referred to as the tension-free vaginal tape or TVT operation. The mid-urethral sling procedure is a minimally invasive surgical operation that involves the placement of synthetic mesh tape to support the urethra and prevent stress incontinence. The Mid-urethral slings have good long-term success rates of 80-85%. These operations can be performed in combination with other procedures such as surgery for prolapse. The two types of mid-urethral slings most commonly used are the retropubic sling (TVT) and trans-obturator sling (TOT).
What happens during surgery?
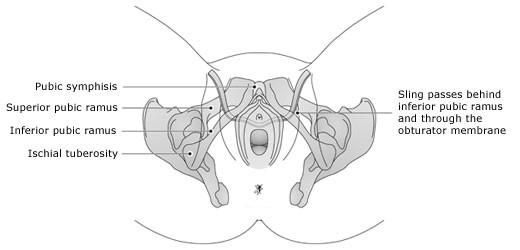
Women can comfortably have the operation with local, regional or general anaesthesia. A small incision is made in the vagina just below the urethra. If you have a retropubic TVT, two tiny incisions will also be made just above your pubic bone. If a TOT is performed, additional tiny incisions are made in your groin on each side. The sling is positioned under your urethra to provide lift and support. This operation takes approximately 20 minutes to perform. Most women return home within 24 hours of the operation.
The illustrations below demonstrate the TVT operation. Small incisions are made above the pubic bone and in the vagina below the urethra. A mesh sling is used to re-support the urethra.
The illustrations below demonstrate the TOT operation. Small incisions are made in each groin and in the vagina below the urethra. A mesh sling is used to re-support the urethra.
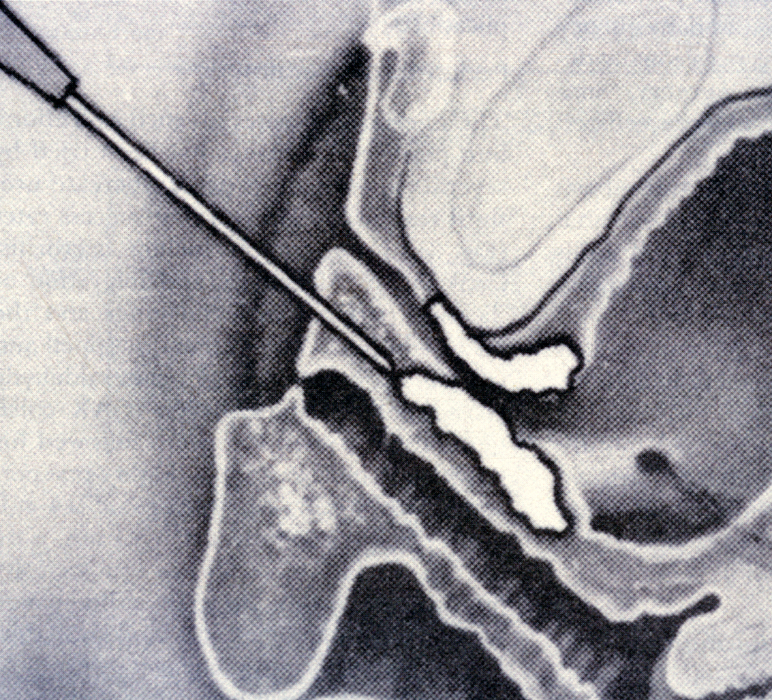
Trans-urethral Bulking Injection
In this procedure, a long acting or permanent filler substance (Bulkamid) is injected into the muscular wall of the urethra under direct vision (urethroscopy). This injection bulks up the lining of the urethral which results in less, or no, urine leakage. Although the cure rate is less after this procedure when compared to the sling or Burch procedures, it is much less invasive, does not require incisions, has a low complication rate and can be performed as a day procedure. About seven out of 10 women who have a Bulkamid injection report significant reduction in urinary incontinence and some women report being completely dry after this surgery. If urinary incontinence returns the same procedure may be repeated (“top-up” injection) or an alterative treatment may be chosen.
Trans-urethral bulking injections are usually recommended for women who are not medically fit for whom more invasive surgery or anaesthetic is not recommended. It is also used for women have a very scarred and rigid urethra (usually from previous surgery). This surgery may be recommended for women who continue to leak after other incontinence surgery.
This illustration shows the bulking material being injected around the urethra, this bulks up the lining of the urethral and reduces or stops urinary loss.
 Dr Carey will be happy to answer any questions you may have and can give more specific advice. Before deciding to have surgery, you should read carefully all the information about your operation and consider obtaining a second opinion.
Dr Carey will be happy to answer any questions you may have and can give more specific advice. Before deciding to have surgery, you should read carefully all the information about your operation and consider obtaining a second opinion.If you experience complications after you leave hospital, contact Dr Carey or the nursing staff on 1 West at the Epworth Freemasons Hospital for advice. In an emergency you may attend the Royal Women’s Hospital, Parkville or Epworth Hospital, Richmond emergency department or attend your closest hospital emergency department.